Living with Paraplegia: Cures, Therapies, Exercises, and More
If you or a loved one is a paraplegic, it is important to learn about the condition and how to live with it.

If you or a loved one is a paraplegic, it is important to learn about the condition and how to live with it.

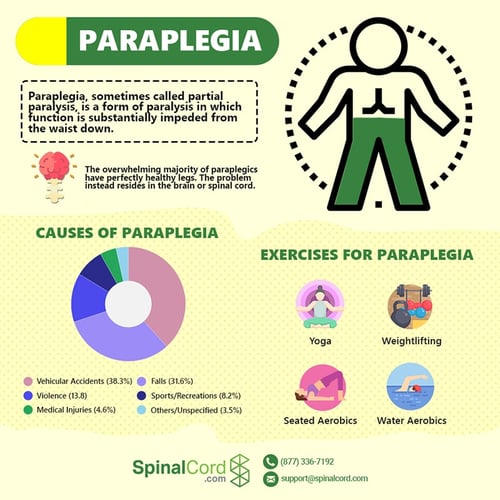
Paraplegia, sometimes called partial paralysis, is a form of paralysis in which function is substantially impeded from below the level of injury. Most people with paraplegia (often referred to as paraplegics) have perfectly healthy legs. Instead, the problem resides in either their brain or spinal cord, which cannot send or receive signals to the lower body due to an injury or disease.
Like other forms of paralysis, paraplegia symptoms can vary significantly from one person to the next. While the stereotype of a paraplegic is of someone in a wheelchair who cannot move his or her arms or legs, cannot feel anything below the level of injury, and cannot walk, paraplegics actually have a range of capabilities that may change over time, both as their health evolves and their physical therapy helps them learn to work around their injuries.
Paraplegia is almost always the result of damage to the brain, spinal cord, or both. In most cases, spinal cord injuries to the thoracic, lumbar, or sacral spinal cord are to blame. When these injuries occur, signals cannot travel to and from the lower regions of the body, and the body is prevented from sending signals back up the spinal cord to the brain.
Thus, paraplegics not only struggle with movement below the level of injury; they also experience extensive loss of sensation. This sensation loss varies from a feeling of tingling or reduced feeling below the level of injury to a complete inability to feel anything below the level of injury.
Some injuries produce temporary paralysis in one or both legs. Even a broken leg can look like paraplegia in the right circumstances, as can the aftermath of a seizure, allergic reaction, and some surgical compilations. Consequently, doctors should not be quick to diagnose paraplegia immediately after an injury. Instead, it can take anywhere from a few hours to several days to diagnose this condition. Your doctor will need to look at your brain and/or spinal cord to see if there are damaged nerves or tissue that impede the ability of signals to travel to and from the legs. Those tests might include:
While paraplegia is typically characterized by the paralysis of the legs, there are different types of paraplegia where the symptoms can vary in severity. Some of types of paraplegia include:
There may be occasions where paraplegia does not fully affect both legs. For example, one leg may be fully paralyzed, while the other has limited or even normal function. This is sometimes known as “incomplete paraplegia,” and can be the result of many different conditions.
In some cases, a case of complete paraplegia may develop into a case of partial paraplegia following rehabilitation therapy for paraplegia. On the other hand, a degenerative condition may cause a case of incomplete paraplegia to become complete paraplegia as symptoms progress.
When some functionality remains in either leg, it may also be referred to as paraparesis, though there is some debate as to whether it should be referred to as such.
This is when the paraplegic retains no feeling or function in their legs whatsoever. A complete paraplegic is unable to use both legs and may experience other issues, such as a loss of bladder/bowel control.
This is common with complete spinal cord injuries in the thoracic and lumbar regions of the spine. Injuries to the cervical region of the spine are more likely to cause quadriplegia (paralysis of the arms and legs).
The primary difference between complete and incomplete paraplegia is whether the paraplegic retains some (or most) of their ability to use or feel either leg. Where a complete paraplegic might not have any functionality or sensation in both legs, a case of incomplete paraplegia may leave the paraplegic with some sensation or motor control.
The National Institute of Neurological Disorders and Stroke (NINDS) defines hereditary spastic paraplegia (or HSP) as “a group of inherited disorders that are characterized by progressive weakness and spasticity (stiffness) of the legs.”
Symptoms of hereditary spastic paraplegia include:
This is a variation of paraplegia that can be inherited from a parent, so it is important to know if any family members have the condition. If there is a history of HSP in the family, then that is a definite risk factor for hereditary spastic paraplegia.
HSP is typically diagnosed via a neurological examination to rule out other conditions that may cause the same symptoms.

Some people may get paraplegia and quadriplegia confused because the two terms are so similar. The major difference between paraplegia vs quadriplegia is that:
Both conditions are typically the result of injuries or diseases affecting the brain and spinal cord. In the case of spinal cord injuries, damage to the cervical spine (i.e. the neck bones) is more likely to result in quadriplegia than injuries lower down on the spine.
The overwhelming majority of paraplegics have perfectly healthy legs. The problem instead resides in the brain or spinal cord. The spinal cord is akin to the body's relay system, sending signals down into the body from the brain and relaying signals from the body to the brain. The brain processes and makes sense of these signals, before sending important information about how to react and feel down the spinal cord and back to the body.
When either the brain or spinal cord do not work properly, these signals may be weak or nonexistent. Consequently, spinal cord injuries (SCIs)—which affect more than 200,000 Americans, with more than 2,500 new cases each year—are the leading cause of paralysis, including paraplegia. According to data from the National Spinal Cord Injury Statistical Center (NSCISC), the leading causes of spinal cord injuries include:
Most spinal cord and brain injuries are traumatic in nature, which means they result from a sudden blow to the area, usually due to an accident. Some injuries, though, are non-traumatic, and usually attributable to diseases or genetic anomalies. A few other causes of paraplegia include:
While paraplegia is usually the result of a disease or accidental injury (meaning they can happen to anyone), there are certain risk factors that increase your chances of becoming paraplegic. It should be noted that a risk factor is not a cause of paraplegia, it is simply something that is common among paraplegics or may contribute to a paraplegia-causing injury or disease.
Here is a shortlist of common paraplegia risk factors:
According to the National Spinal Cord Injury Statistical Center (NSCISC), “78% of new SCI cases are male.” Since SCI is a common cause of paraplegia, this makes men more likely to become paraplegic than women.
NSCISC data shows that the average age of a person who suffers a spinal cord injury is now 43 (up from 29 a few decades ago). Senior citizens with osteoporosis and other conditions affecting bone health are also more likely to suffer a severe SCI during a fall or other accident.
Certain jobs and sports increase the likelihood of severe impacts to the head or spinal column—which can increase the risk of becoming paraplegic. Examples include Law enforcement, construction work, boxing, football, diving, and hockey.
Certain inherited nerve diseases and other conditions can be contributing factors to brain and spinal injuries that increase the risk of developing paraplegia.
Paraplegia is a variable condition. The same person might experience symptoms that change over time, or that even alter from one day to the next. Proper therapy can greatly affect the prognosis and improvement of the disease, but many outcomes appear random. There is much we do not yet understand about the brain and spinal cord, so doctors are not yet sure why some people spontaneously recover while others languish without progress even with intense therapy.
In some cases, symptoms improve as swelling in the injured area dissipates. Treatment of infection and disease-related processes may also reduce or reverse symptoms, or slow the improvement of paraplegia. Thus the best source for information on how paraplegia might affect your life is your doctor. Know, however, that even the best doctors cannot be certain about the prognosis, and you should not allow even a grim prognosis to undermine your motivation to keep working toward recovery.
Some of the most common effects of paraplegia include:
To accurately diagnose the type of paraplegia a person is experiencing and its cause, a doctor will typically perform an in-depth examination. These examinations are necessary to identify the best paraplegia therapy and exercise regimen for the patient to increase their life expectancy and promote wellness.
Diagnosing paraplegia may involve:
Once the diagnosis is complete, a doctor may begin recommending a paraplegia exercise regimen and therapy schedule to help the patient cope with paraplegia.

Paraplegia is a life-altering condition for many—whether they were born with a hereditary condition that caused a slow change or suffered a sudden illness or accident that caused paraplegia.
Learning how to live with paraplegia is important for the paraplegic and for those around them. When a loved one loses function in their legs, it requires everyone they know to adapt.
There are many medical complications that paraplegia can cause beyond removing the ability to walk. Not being able to stand up and move can cause a variety of additional conditions that can range from being mildly inconvenient and/or painful to being potentially life-threatening.
Here are some of the common medical complications that can arise from paraplegia:
The inability to move can cause sores to develop on the legs or buttocks. To prevent this, it is important to engage in paraplegia exercises and to adjust positions regularly if possible.
Urinary retention is a common side effect of paraplegia since the link between the brain and the nerves controlling the bowels and bladder is damaged. This can also lead to urinary tract infections (UTIs) as bacteria may sit in the urinary tract and infect the bladder. Antibiotics can help clear UTIs, while indwelling catheters or intermittently using a catheter to drain the urine can help prevent urine retention.
Living with paraplegia can be extremely difficult. It is common for paraplegics to become extremely depressed following a paraplegia-causing injury or illness. It is important for paraplegics to find support—both from loved ones and from support groups.
Another common side effect of not being able to move freely is the development of circulatory disorders. Engaging in exercise or finding an occupational therapy specialist can help.
A loss of function and feeling in the sexual organs is extremely common among paraplegics. Many people assume that paralysis eliminates the possibility of sex. However, being paralyzed from below the level of injury does not have to be the end of your sex life.
For men, it may still be possible to achieve erections using “reflex triggers” (contact-based stimuli to erogenous zones—like the phallus—on the male body). Reflex triggers using penile vibrators can help paralyzed men achieve an erection and even ejaculation in some cases —although some may not be able to if the sacral spinal nerves themselves are damaged.
For women, a loss of sensation in the vagina can make it difficult to achieve lubrication and orgasm. Tiffiny Carlson, an SCI survivor who has guest blogged for spinalcord.com, noted the importance of experimenting to find alternative erogenous zones to stimulate pleasure from sexual intercourse. It can also help to use “bedroom aids” such as lube to enhance intercourse.
For both men and women, finding alternatives to standard intercourse (such as engaging in more extended foreplay) can help couples maintain an active and healthy sex life after paraplegia.
Many people with paraplegia look for a miracle “paraplegia cure” to alleviate their condition. While there is no known cure for paraplegia in all its forms, there are things that people can do to speed their recovery and even potentially restore some of their legs’ functionality.
Paraplegia recovery can be a long and difficult process as paraplegics learn to cope with their paraplegia symptoms. There are numerous steps to recovering from paraplegia—steps that may change depending on the cause and severity of the condition.
Some basic steps to paraplegia recovery include:
As noted earlier, some (or all) of these steps may change. For any paraplegia recovery plan, it is important to consult a qualified physician before starting any therapy regimen.
Every patient is different, and therapy that works well for you might not work for another person. Generally speaking, intensive therapy gives you the best chance at recovery, particularly when you begin receiving therapy immediately after the injury. Spinal Cord Injury Model Systems offer comprehensive and highly rated therapy, so if such a facility is near you, consider moving your recovery to that location.
Some therapy options include:
Physical therapy can prove to be an excellent tool for helping paraplegics improve their health and even help alleviate some paraplegia symptoms. Some paraplegia exercises that paraplegics can benefit from include:
Many SCI survivors and paraplegics can benefit from the gentle stretching exercises involved in yoga activities, as they help to stretch unused muscles and prevent atrophy. Breathing exercises found in this particular type of paraplegia exercise can also help those who have difficulty breathing because of the side effects of a brain or spinal cord injury.
Weightlifting is an exercise for paraplegics that allows them to heavily work on their muscles, preventing atrophy while actively increasing physical strength and health. However, weightlifting for SCI survivors and paraplegics should be conducted under the watchful eye of a physical therapist to avoid overworking muscles and causing further injury.
As odd as it might sound, water aerobics can be exceptionally beneficial as a paraplegia exercise. The water helps support the weight of the body while allowing paraplegics to get out of the chair and stretch limbs that are otherwise difficult to exercise. Proper support and supervision is a must for this type of physical rehabilitation exercise.
There are a number of different aerobic exercises for people that can be done from inside of a chair. The benefit of this paraplegia exercise is that it can be done from virtually anywhere—making it easy to engage in even without visiting a spinal cord injury rehabilitation center.
Some facilities specialize in providing spinal cord injury rehabilitation to help people who are paralyzed lead active and healthy lives. These spinal cord injury rehabilitation centers are scattered throughout the country, so SCI survivors may need to ask their physician or a local SCI advocacy group to find a facility near them.
Those seeking acute inpatient rehab may want to begin by researching the Spinal Cord Injury (SCI) Model System, and the individual Model System Centers around the country.
One example of a spinal cord injury rehabilitation center could be an activity-based therapy center. These facilities focus on providing therapeutic activities and exercises to help members of the SCI community improve their health and body function. You can find a map of activity-based therapy centers here.
People who live with paraplegia resulting from a spinal injury or spinal nerve damage frequently need assistance in adjusting to life after an SCI. Finding and joining SCI community groups can help paraplegics by providing more than just resources and advice—they also provide an outlet for talking about whatever challenges or issues that SCI survivors and their loved ones have to deal with.
SCI community resources can be found online through social media platforms like Facebook or Twitter, by asking physical therapy specialists, or by looking at lists of SCI support groups like this one.
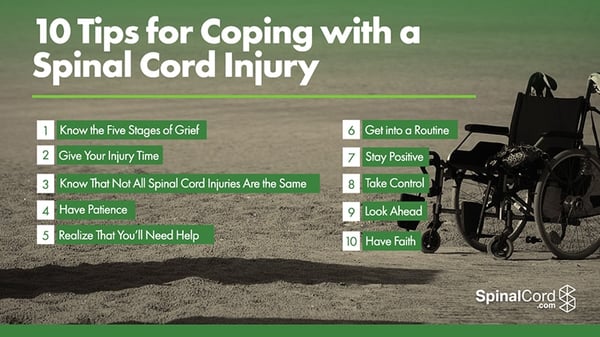
Spinal cord injuries are traumatic for patients and their families. They cause disruptive changes to every aspect of your life and there is a lot of new information to navigate and understand. Our experts have collected everything in one place to help you learn more about your injury, locate doctors and treatment centers, find financial support, and get assistance navigating your next move.
Sponsored by Tampa personal injury lawyers at Swope, Rodante P.A. a Florida law firm located at 1234 E 5th Ave, Tampa, FL 33605.
The information provided by SpinalCord.com is not a substitute for professional medical advice, diagnosis, or treatment, see Disclaimer Policy.